The penis is the main component of the genitourinary tract of males, as it ensures a wide range of vital physiological functions, including erections, ejaculation, and micturition.
This organ has a complex anatomy that allows it to perform different functions, such as size variation between the state of erection and flaccidness.
In this article we will comprehensively cover the anatomy of the penis and see how each structure offers different physiological functions
The Anatomy Of The Penis-Overview
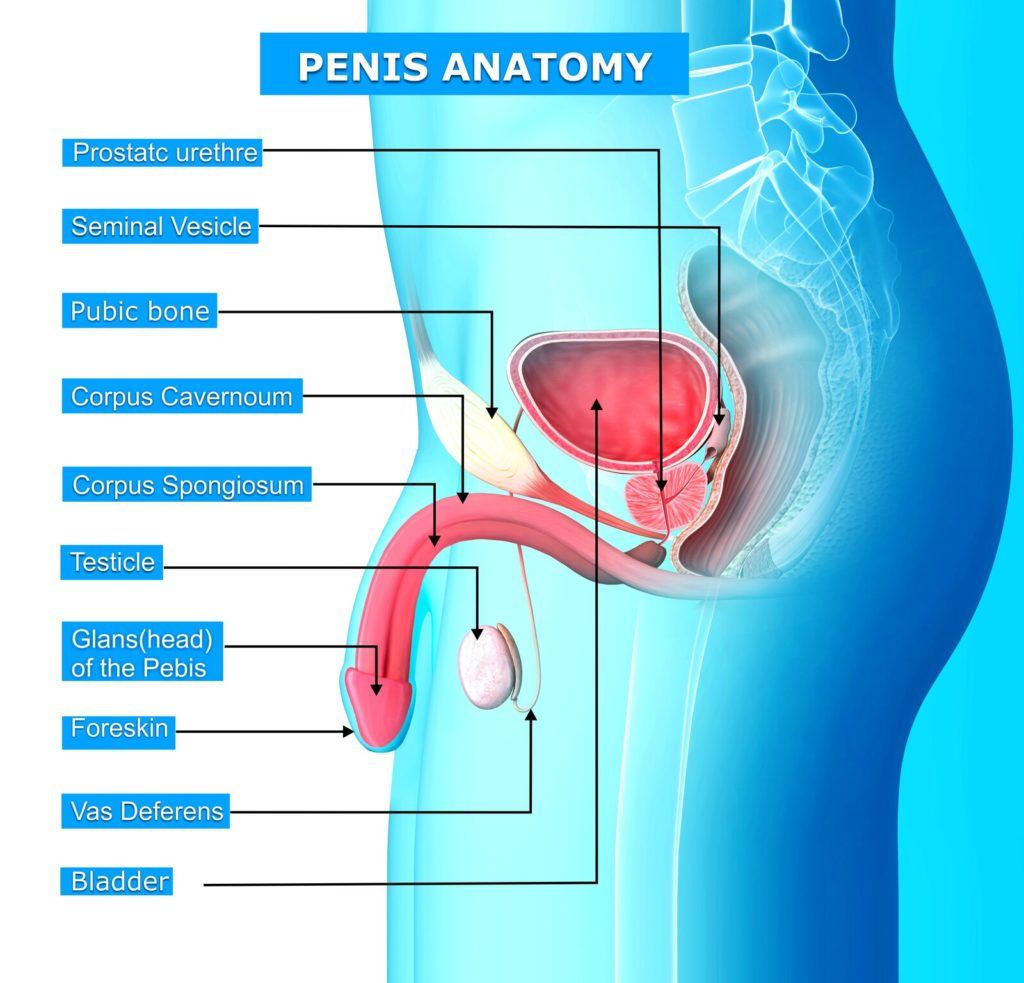
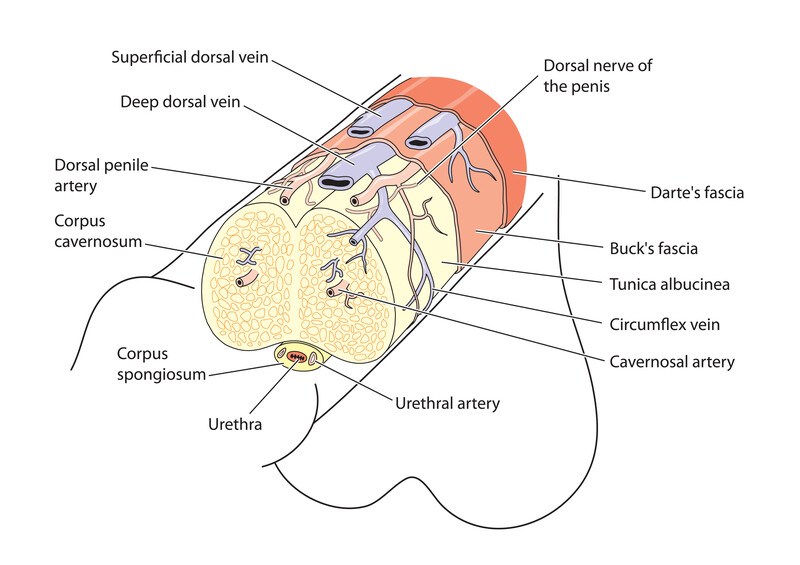
The penile shaft has 3 erectile columns (2 corpora cavernosa and one corpus spongiosum), blood vessels, nerve endings, and lymphatic circulation. (1)
All of these structures are covered by the skin.
An erection is mediated by the corpora cavernosa that contains erectile tissue, as well as a few elastic fibers found in the tunica albuginea.
In the upcoming sections, we will detail each component of the penile tissue.
Penis Anatomy -The Glans
The penis glans is a cap expansion of the corpus spongiosum that’s molded on the distal ends of the corpora cavernosa.
The glans will then extend on the upper and lower surfaces of the corpora cavernosa. The term glans was derived from the Latin word for ‘acorn’, which means a smooth oval nut.
In the central end of the glans, there is an opening of the urethra that allows semen and urine to exit the body, which is referred to as the meatus.
At birth, the glans of the penis will be attached to the foreskin, which will separate from the glans until the skin becomes fully retractile.
This process is long and can take up to 18 years to fully separate.
In circumcised children, the majority of the foreskin is removed, leaving the glans exposed and increases the risk of some infections at the meatus (urethra opening) level.
However, uncircumcised children are also prone to bacterial overgrowth, hence the need for daily cleaning of the glans and meatus. (2)
Penis Anatomy-The Urethra
Gross Anatomy
The spongy part of the urethra forms during the tubularization phase (embryological phase) under the influence of dihydrotestosterone.
For the anatomy of the urethra, it originates from the bladder neck and ends at the meatus on the glans penis.
The length of the urethra varies between males but it ranges between 15-25 cm with an “S” curved shape when viewed from the sides.
Anatomists divide the urethra into 3 segments:
- Prostatic urethra
- Membranous urethra
- Spongy urethra
Prostatic Urethra
As the name implies, this segment of the urethra goes through the prostate after originating from the bladder neck to finally end at the membranous urethra.
The prostatic urethra is supported superiority by the bladder and inferiority by the perineal membrane and the sphincter urethrae externus muscle. (3)
It traverses the prostate in an area that’s prone to benign prostatic hyperplasia (BPH), which compresses the prostatic urethra and causes all the signs and symptoms associated with BPH.
As for the posterior side of the prostatic urethra, it houses the urethral crest that’s laterally limited by the prostatic sinuses to drain the surrounding glands.
This crest contains the seminal colliculus, or verumontanum, which is the area where the ejaculatory ducts and the opening of the prostatic utricle meet.
Membranous Urethra
Relative to the other segments, the membranous urethra is the shortest, spanning from the apex of the prostate to the bulb of the penis. The membranous urethra is invested in the perineal membrane, as well as the external urethral sphincter.
Spongy Urethra
This portion of the urethra was given this name because it runs along the corpus spongiosum.
Typically, experts divide this portion into:
- The pendulous urethra
- Bulbar urethra
Vasculature and lymphatic drainage
The vascular supply of the urethra is somewhat complex, with the prostatic urethra being supplied by the inferior vesical artery that branches to penetrate the prostate and the bladder.
The membranous and the bulbar urethra are supplied by the bulbourethral artery, whereas the pendulous urethra gets its vascularization from the deep penile artery.
Generally speaking, the veins mirror the arteries in draining different portions of the urethra.
As for the lymphatic drainage, the penile urethra drains to the deep and superficial inguinal nodes.
Anatomy of The Penis-The Corpus Cavernosum
The corpus cavernosum contains the spongy erectile tissue that mediates an erection.
Each corpus cavernosum has an artery running along its middle axis that’s properly named the cavernosal artery, which initiates erections when blood flow runs through.
There are muscles that support the dynamic changes of corpus cavernosum and the penis during erection and ejaculation.
The relaxation of these muscles will send signals to the brain to start the process of an erection by pumping blood inside the corpora cavernosa, creating a pressure that expands the penile tissue and blocks the drainage of blood of the veins.
Once the muscles contract again, blood flow will moving through the penis, and the veins restore their function.
The Corpus Spongiosum
The corpus spongiosum is a mass of erectile tissue that’s located under the corpus cavernosa. This entity contains approximately 90% of the blood volume that’s redirected to the penis during physiological erection.
As you can see in the figure above, the corpus spongiosum houses the urethra and extends to form the glans penis.
The physiology of the penis
As we mentioned earlier, the spongy tissue of the penis can expand when blood rushes into the penile arteries, leading to an erection.
As the expansion occurs, the veins will be blocked to prevent blood drainage, thus maintaining the erection.
The process of tissue expansion creates a gradient between systematic blood pressure and penile pressure, where the latter exceeds the pressure of the former, blocking arterial flow to the penis.
This physiology is what allows the penis to get erect and is mediated by the parasympathetic nervous system and a crucial molecule known as nitric oxide (NO), which promotes the relaxation of smooth muscles found in the vessels of the penis to allow for blood flow. (4)
In some cases, this entire process can get disrupted, leading to a classic condition referred to as erectile dysfunction (ED).
Penile Anatomy-Erectile Dysfunction
Erectile dysfunction, or ED, is a common medical condition that results in an inability to get or maintain a penile erection for the duration of sexual intercourse.
According to the American Journal of Medicine, ED affects more than 18 million Americans, which translates to approximately 18.4% of the male population.
Unfortunately, there are several causes that may lead to ED. This complicates the diagnostic and therapeutic approaches.
Causes of Erectile Dysfunction
Numerous conditions can lead to ED, including vascular problems, neurological abnormalities, and psychological stress.
Pathophysiology of Erectile Dysfunction
Regardless of the many medical conditions that may lead to erectile dysfunction, the final result is usually the same. All patients deal with the interruption of normal blood flow through the penile arteries.
Consequently, they can no longer get and/or maintain an erection.
ED results from the disruption of one or more of the following components:
- Smooth muscle damage
- The absence of vasodilators (e.g., nitric oxide)
- Partial obliteration of the penile blood vessels (i.e., atherosclerosis)
Unfortunately, each of these mechanisms is different, hence the need for various therapeutic approaches.
Anatomy of the Penis-Conclusion
The penis is a fascinating piece of architecture that houses complex structures to maintain its anatomical integrity and ensure its vital physiological roles.
This article covered the basic concepts of penile anatomy without addressing some complicated topics, such as the embryological origins of different tissues or the neuroendocrine physiology that facilitates erection and ejaculation.
However, we hope this overview helped you appreciate the structural complexity of the penis and how each component plays a crucial role in the physiology of the male reproductive system.